A 19-year-old, male working as a farmer presented with high-grade fever > 100° F, myalgia, and anemia for 2 months duration. Treated at local hospitals for 6-8 weeks and was referred to us for further management. 15 days later he started developing joint pains involving large and small joints. He did not suffer from any arthritis in the past. No history of fever, sore throat, allergic rashes, bites, or stings in the recent past. He did not have any history of weight loss, cough, hemoptysis, abdomen pain, breathlessness, chest pain, sweating, back pain, urethral discharge, burning urination, or palpitations. No similar complaints in family or contacts. No history of tuberculosis, autoimmune diseases, or recent vaccination.
Examination revealed mild pallor without any lymphadenopathy, splenomegaly, crepts, or ronchi. Initial evaluation revealed he had anemia with hemoglobin of 8.3gm%, WBC count of 20,700 cells/cumm, and PMN of 89%. Peripheral smear was microcytic and hypochromic, neutrophilic leukocytosis with pencil-shaped cells. His creatinine was 0.8mg/dL, however, ultrasonography showed bulky kidneys with raised echotexture. Urine routine examination, Urine for AFB and microscopy were normal. Serum albumin was 2.7g/dL - s/o malnutrition vs acute phase reactant. The Widal test was positive at 1: 160. Brucella and Rheumatoid factor were negative. Malaria Rapid and QBC smear were negative. A blood culture was sent.

He was started on broad-spectrum antibiotics along with atypical coverage. Day 5 was completed, fever was recurring. Over the next couple of days, he developed left knee joint swelling, associated with effusion. ROM was restricted along with local redness. USG-guided effusion was tapped and sent for analysis. Effusion was turbid with 200 cells, predominantly neutrophils, and few lymphoid cells. Fluid biochemistry was s/o acute inflammatory exudate. The synovial fluid culture was negative. Blood culture was negative on day 7.
The fever was persistent. Further workup was done towards ANA Profile, Vasculitis panel, and Echocardiogram for infective endocarditis showed no vegetation. GeneXpert MTB on Urine, Synovial fluid, and Sputum were negative. Fundoscopy showed no evidence of choroid tubercles and uveitis. CECT Thorax, abdomen, and pelvis with oral and IV contrast were unremarkable.
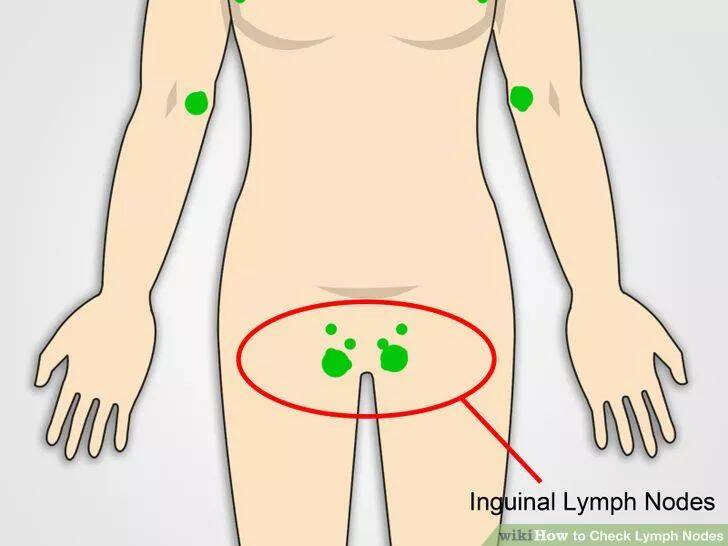
4 weeks passed by, fever was recurrent and persistent. In 5th week patient developed Right Inguinal Lymphadenopathy. FNAC was reported to be reactive lymphadenitis. Excision biopsy of the same was negative for TB, Granulomas, and Malignancy. VDRL was negative, and CSF analysis was also normal.
As all workup was negative, IGRA was planned. However, due to economic constraints, the patient was unwilling for the test. Finally, Poncet's was considered a diagnosis of exclusion, and anti-tubercular medications were started. Weight band adjusted ATT (anti-tubercular therapy under NTEP regimen) was started. The patient felt significant improvement in general health, febrile episodes were absent by 48 hours. Appetite improved. CRP showed a decreasing trend.
Blood was transfused in view of anemia. Iron supplements and multivitamins were started. After 4 days of afebrile episodes, the patient was discharged with a diagnosis of Poncet's disease.
Poncet's disease is an unusual manifestation of active or latent tuberculosis manifesting as reactive arthritis. It's usually a diagnosis of exclusion. In developing countries like India, Tuberculosis poses immense challenges to physicians because of its myriad presentations.
Case Highlight: Dr. Chetan K Ganteppanavar, Director and Consultant Physician at Kalpana Multi Speciality Clinic, Hubli, managed a challenging case of Poncet's disease. The patient, a young farmer, presented with persistent fever and joint pain. Extensive investigations ruled out other conditions, and despite negative TB tests, Poncet's disease was diagnosed based on clinical judgment. The patient responded remarkably well to ATT, highlighting the importance of considering TB in differential diagnoses, especially in endemic areas.
Conclusion: Poncet's disease, though rare, should be considered in patients with unexplained polyarthritis, particularly in TB-endemic regions. Early diagnosis and prompt ATT can lead to complete recovery, underscoring the critical role of clinical acumen in managing such complex cases.
